Chronic pain affects millions of people worldwide, often disrupting daily life and reducing overall well-being. Common pain areas include the shoulder, lower back, knee, and foot and ankle. When standard treatments fall short, Peripheral Nerve Stimulation (PNS) offers a cutting-edge, minimally invasive solution for lasting relief.
What Is Peripheral Nerve Stimulation?
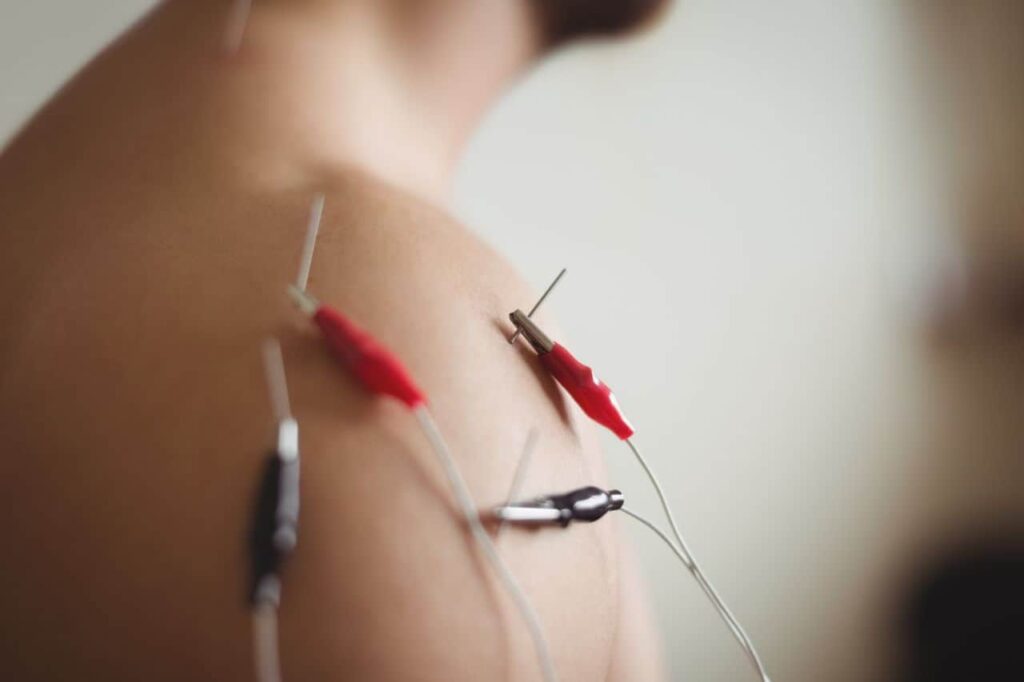
PNS works by targeting the nerves responsible for sending pain signals, interrupting these signals before they reach the brain. This method offers focused pain relief without the need for long-term medications or invasive surgery.
Two Leading FDA-Cleared PNS Systems:
🔹 Nalu PNS System
- How It Works: Thin wire leads are placed under the skin and connected to a small rechargeable device (micro-IPG).
- Benefit: Provides continuous, low-level electrical stimulation to block pain signals without frequent battery replacements.
🔹 SPRINT PNS System
- How It Works: Uses a temporary MicroLead placed near pain-generating nerves.
- Treatment Duration: 60 days.
- Benefit: Offers sustained relief with no permanent implants or medications required.
Proven Effectiveness of PNS
Clinical research highlights the impressive results of PNS therapy:
- ✅ Pain Relief: Up to 70–80% of patients report significant reductions in pain intensity and frequency.
- ⏳ Long-Term Benefits: Relief may last up to 14 months post-treatment.
- 💪 Functional Improvement: Enhanced mobility and reduced interference in daily activities.
- ⚠️ Low Risk: Most side effects are mild (e.g., minor skin irritation). Serious complications and device failures are rare.
Common Nerve Targets for PNS
Over 20 peripheral nerves are commonly treated with PNS, depending on the pain location:
- Upper Body: Suprascapular, axillary, radial, median, ulnar nerves
- Lower Body: Sciatic, femoral, tibial, peroneal, genicular nerves
- Trunk/Back: Medial branch, intercostal, and cluneal nerves
These targeted approaches make PNS effective for conditions like:
- Neuropathic pain
- Phantom limb pain
- Postoperative pain
- Chronic musculoskeletal pain
What to Expect During the PNS Procedure
- Initial Consultation: Assessment includes medical history, physical exam, and sometimes diagnostic nerve blocks or trial stimulation.
- Lead Placement: Performed with ultrasound or fluoroscopic guidance for precise targeting and reduced risk of complications.
- Recovery and Care: Patients receive instructions for care and can often resume normal activities shortly after the procedure.
Safety Guidelines & Best Practices
The American Society of Pain and Neuroscience classifies PNS as a low-to-intermediate risk therapy. With proper screening, imaging guidance, and follow-up care, risks like bleeding or infection remain minimal. In some cases, a psychological evaluation may be recommended to improve overall outcomes, especially in complex chronic pain cases.
Insights from Recent Research
New studies continue to validate the benefits of PNS:
- Significant improvements in mobility, function, and quality of life
- Strong results in post-surgical pain, including after knee replacements
- Effectiveness across diverse patient populations in real-world settings
These findings support using PNS earlier in treatment plans—not just as a last resort—especially when aiming to prevent chronic pain after surgery or injury.
Is PNS Right for You?
You might be a good candidate for Peripheral Nerve Stimulation if you:
- Have not responded well to conventional pain therapies
- Prefer a minimally invasive and reversible treatment
- Want a drug-free option for managing chronic pain
Final Thoughts
Peripheral Nerve Stimulation is transforming how we manage chronic pain—providing targeted, long-lasting relief without the side effects of medications or invasive surgery. If you’re struggling with pain that hasn’t responded to other treatments, talk with your healthcare provider about whether PNS could be the breakthrough you’ve been waiting for.